Researchers Investigate a More Effective Technique for Preserving Ovarian Tissue
Posted March 13, 2019
The technique is indicated for patients undergoing chemotherapy or radiation therapy, treatments that can cause infertility
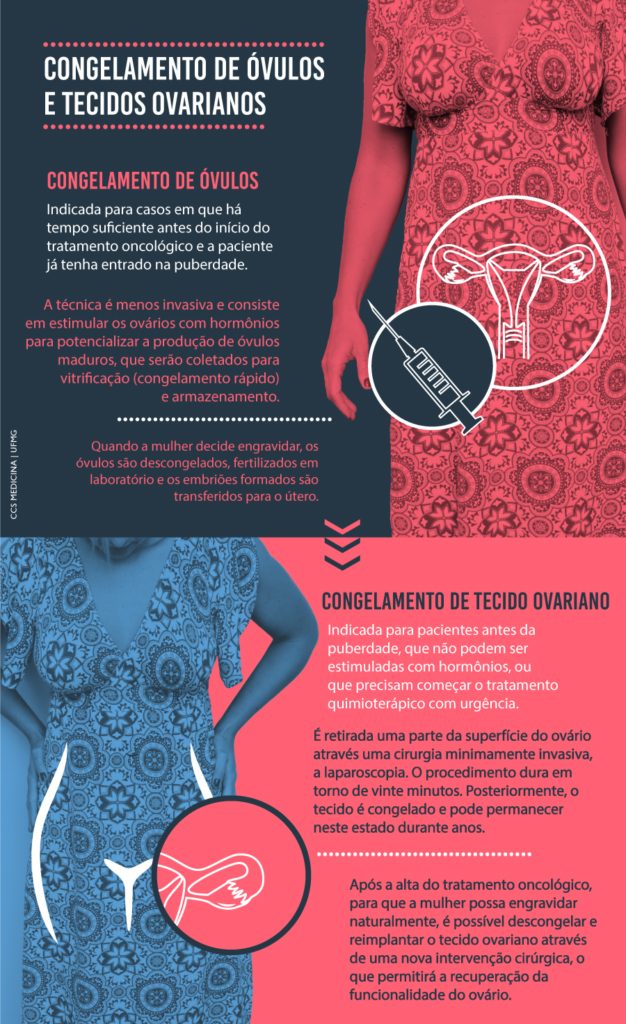
Ovarian tissue freezing is a promising current option for women who dream of having children after undergoing cancer treatment. Unlike egg freezing, this technique allows recovery of ovarian function not only in terms of fertility, but also in terms of hormone production. To improve the results obtained after transplantation of frozen ovarian tissue, faculty and researchers affiliated with the UFMG School of Medicine and the National Institute of Science and Technology in Hormones and Women’s Health (INCT Hormona) have been developing more effective preservation techniques.
Improvements are already being observed in animal models, and these new techniques will be tested in human tissue as early as the first half of 2019. According to Fernando Reis, a professor at the Department of Obstetrics and Gynecology and one of the investigators involved in the project, the practice of ovarian tissue freezing is already used in reproductive medicine, but there is still much room for improvement.
Tissue freezing is indicated for patients who will undergo chemotherapy or radiation therapy—treatments that can cause infertility. Thus, the more tissue preservation can be achieved, the better. With this technique, ovary fragments that have been frozen can be transplanted back into the patient’s body once the cancer has been cured. “The tissue will thus regenerate, and the patient regain her ability to produce hormones, ovulate, and become pregnant spontaneously or through assisted reproduction,” explains Fernando.
Because this tissue is highly sensitive, the research group is focusing on a technique that uses novel cryoprotectant substances to prevent possible damage caused by exposure to extremely low temperatures. The study compares two freezing techniques: slow and ultrarapid freezing (so-called vitrification), with and without the use of synthetic polymers, which are chemicals that might protect cells even further.
The investigators have been testing these techniques on monkey and cow ovaries. According to Professor Reis, these animals were chosen because of a structural and functional similarity with human ovaries. Ongoing trials in cattle are using material donated by meat processing plants. The results should be available later this year.
HUMAN TISSUE
Project co-investigator Jhenifer Kliemchen Rodrigues, a postdoctoral fellow at the Graduate Program in Women’s Health and a guest professor at the School of Medicine, carried out the same tests on monkey ovaries in the United States, with promising results.
The researchers now hope to test the two techniques and the protective effect of synthetic polymers on tissues donated by women who need to undergo treatments such as chemotherapy or radiation therapy, the side effects of which can damage their ovaries.
According to the study protocol, approved by the UFMG Research Ethics Committee, only a small part of the material obtained from each donor will be used to investigate the new freezing techniques. Most will be stored using current gold-standard techniques for future use by the patients.
Additional
reporting from Portal da UFMG.
Copy: Marcela Brito
Photo credit: Carol Morena
Supervisor: Karla Scarmigliat
Editing: Luiz Sérgio Dibe